A STUDY TO ASSESS THE EFFECTIVENESS OF REBOUNDING EXERCISE ON LYMPHEDEMA : Shailendra Mehta *
Abstract
Background : Rebounding is a fantastic exercise for those with Lymphedema, arthritis sufferers and other similar conditions. Lymphedema is a swelling that develops as a result of an impaired lymphatic system.Your lymphatic system has no pump and cannot move fluid on its own. When you jump up and down on a rebounder, or trampoline, you are helping push that fluid throughout your body .The study was aimed at evaluating the effectiveness of rebounding exercise on lymphedic patients. A total of 30 patients those suffers with lymphedema has been taken from govt &private hospital , Udaipur , and the rebounding exercise was practiced for the selected samples. Condition of the lymphedema was analyzed before and after the study. Collected data was analyzed using descriptive and inferential statistics. A high significant On an average, in experimental group, lymphedic patients are having 56.6 % improved where as in control group, on an average, lymphedic patients are having only 6.3 % improved
Conclusion : Rebounding exercise could be an effective vascular rehabilitation training program for vascular remodeling in lymphedema patients
Keywords : Reboundine exercise, lymphedema, vascular rehabilitation
Background:
Lymphedema as defined as the abnormal accumulation of protein-rich fluid in soft tissues, results from a dysfunction of the lymphatic system. This dysfunction can be either a congenital abnormality in the development of the lymphatic system, or a secondary obstruction, destruction, or malfunction of the lymphatic pathway. It is a common and troublesome problem.
Rebounding affects the lymphatic system much like a massage does. The lymphatic system is the metabolic rubbish bin of the body. It rids you of toxins such as dead and cancerous cells, nitrogenous wastes, fat, infections viruses, heavy metals, and other assorted junk cast off by the cells.
Unlike the cardio-vascular system, there is no “pump” driving the fluid round the body. When on the rebounder, the “jump” motion at the top of the jump forces the lymphatic valves to open, the “push” motion closes these valves at the bottom of the jump. This creates a “pump” effect which effectively moves and recycles the lymph and the entire blood supply through the circulatory system many times during the course of the rebounding session, providing a free-flowing system that drains away the potential poisons from our body.
This lymphatic drainage eliminates waste products quickly and efficiently both during and after exercise (lactic acid dissipation)
Get started with a gentle bounce, 2 -3 minutes once or twice each day, with your feet staying on the mat surface – this is called the “health bounce”. If you have balance problems due to inflammation then use the stability bar. Gradually progress to small jumps off the rebounder. At no time, even during vigorous exercise, will your feet leave the mat surface by more than 6 inches.
Methods :
Sample Thirty(30) patients with a diagnosis of primary or secondary unilateral lymphedema of either the upper or the lower limb with observable swelling of the involved limb were the subjects.
None of the subjects received active treatment for lymphedema within the six months period before entering the study.
Exclusion criteria: – active cancer cases, influencing drugs including diuretic, signs of infection in the affected limb (redness, rash, red streaks, hotness, pain), evidence of contraindications to treatment: uncontrolled hypertension, congestive heart failure, renal insufficiency, and venous thrombosis.
Treatment Intervention :
All patients underwent complete physical examination and were evaluated for their eligibility in participating in this study. The scheme of the study was discussed in detail with the patient prior to start. All the patients received six sessions; three sessions weekly (for two weeks) in two points of the study: week 1 and week 7. Then, the patient was instructed to do the same regimen at home for the following 4 weeks (at week 3 and week 9.
The “health bounce” is performed for two to three minutes once or twice a day. In the health bounce, stand on the trampoline and lightly move your heels up and down. Your feet remain in contact with the base. To increase the challenge of the bounce as you progress, move your heels from side to side in a twisting motion.
Assessment and Outcome Measures:
Baseline and demographic data were recorded for each subject and included the age, limb circumference duration of lymphedema, side of the swelling. The follow up measures were recorded at week 12.
Results :
Patient Characteristics Thirty patients with unilateral extremity lymphedema were enrolled in this study.
Treatment Outcomes :
All the recruited patients received the program as designed in the study.
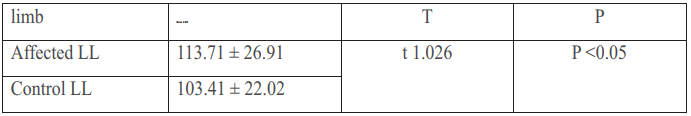
There was a significant difference (p < 0.05) in the circumferential measures of the affected LL (113.71 ± 26.91) as compared to the non- affected control LL(103.41 ± 22.02) was found. This might be explained by the fact that most of our upper limb cases were secondary; either to mastectomy with axillary lymphadenectomy.
Discussion:
The challenge of living life with lymphedema is daunting. The swelling from pooling lymphatic fluid never completely disappears. At times, depending on various factors, it can lessen. There are many ways to help disperse the fluid, but it always returns, and for good reason. When the normal lymphatic flow in the body has been disrupted by the removal of lymph nodes, lymphatic fluid needs somewhere to go, and when it can’t travel, lymphedema sets in.
The lymphatic system is a huge network of tissues and organs that help rid the body of dangerous toxins. Its primary function is to transport lymphatic fluid throughout the body. The lymphatic fluid contains white blood cells specifically designed to fight infection. The lymphatic system is similar to a busy interstate. When there are no obstructions, the lymphatic fluid flows freely in one direction through the circulatory system of veins and capillaries. The lymphatic vessels are connected to lymph nodes, which help filter lymphatic fluid. Everything is designed to work perfectly. The tonsils, spleen, adenoids and thymus are all part of the lymphatic system. Throughout the body, there are hundreds of tiny lymph nodes. Just like a busy interstate, this system is set up to keep the lymphatic fluid moving Dave Scrivens, Certified Lymphologist, which was published in the Well Being Journal Vol. 17, No. 3. In his article, Mr. Scrivens says, “The body has a built-in need for activation. The lymph system, for example, bathes every cell, carrying nutrients to the cell and waste products away. Yet the lymph is totally dependent on physical exercise to move. Without adequate movement, the cells are left stewing in their own waste products and starving for nutrients, a situation that contributes to arthritis, cancer and other degenerative diseases. Vigorous exercise such as rebounding [jumping on a therapeutic mini-trampoline] is reported to increase lymph flow by 15 to 30 times. Also, bones become stronger with exercise. Vertical motion workouts such as rebounding are much different and much more beneficial and efficient than horizontal motion workouts, such as jogging or running. The lymph fluid moves through channels called “vessels” that are filled with one-way valves, so it always moves in the same direction. The main lymph vessels run up the legs, up the arms and up the torso. This is why the vertical up-anddown movement of rebounding is so effective to pump the lymph.
Dr. Scrivens also says, “The lymphatic system is the metabolic garbage can of the body. It rids you of toxins such as dead and cancerous cells, nitrogenous wastes, infectious viruses, heavy metals, and other assorted junk cast off by the cells. The movement performed in rebounding provides the stimulus for a free-flowing system that drains away these potential poisons. Unlike the arterial system, the lymphatic system does not have its own pump. It has no heart muscle to move the fluid around through its lymph vessels. There are just three ways to activate the flow of lymph away from the tissues it serves and back into the main pulmonary circulation. Lymphatic flow requires muscular contraction from exercise and movement, gravitational pressure, and internal massage to the valves of lymph ducts. Rebounding supplies all three methods of removing waste products from the cells and from the body
REFERENCES :
1. Földi, M, E Földi, S Kubik: Textbook of Lymphology: For Physicians and Lymphedema Therapists. Urban and Fisher, San Francisco, CA, 2006.
2. Cormier, JN, RL Askew, KS Mungovan, et al: Lymphedema beyond breast cancer: A systemic review of cancer-related secondary lymphedema. Cancer 116 (2010), 5138-5149.
3. International Society of Lymphology: The diagnosis and treatment of peripheral lymphedema: 2009 consensus document of the International Society of Lymphology. Lymphology 42 (2009), 51-60.
4. National Lymphedema Network: Position statement of the National Lymphedema Network: The diagnosis and treatment of lymphedema. Accessed A p r i l 1 0 , 2 0 1 2 , a t h t t p : / / www.lymphnet.org/pdfDocs/nlntreatment.pdf.
5. Deo, SVS, S Ray, GK Rath, et al: Prevalence and risk factors for development of lymphedema following breast cancer treatment. Indian J. Cancer 41 (2004), 8-12.
6. Armer, JM, BR Stewart: Post-breast cancer lymphedema: Incidence increases from 12 to 30 to 60 months.Lymphology43 (2010),118127.
7. Ronka, RH, MS Pamilo, KAJ von Smitten, et al: Breast lymphedema after breast conserving treatment. Acta Oncol. 43 (2004), 551-557.
8. Rinehart-Ayres, M, K Fish, K Lapp, et al: Use of compression pumps for treatment of upper extremity lymphedema following treatment for breast cancer: A systematic review. Rehab. Oncol. 28 (2010), 10-18.
9. Moseley, AL, CJ Carati, NB Piller: A systematic review of common conservative therapies for arm lymphoedema secondary to breast cancer treatment. Ann. Oncol. 18 (2007), 639-646.
10. Olszewski, WL, P Jain, G Ambujam: Tissue fluid pressure and flow in the subcutaneious tissue in lymphedema-hints for manual and pneumatic compression therapy. Phlebolymphology 17 (2010), 144-150.
11. Adams, KE, JC Rasmussen, C Darne, et al: Direct evidence of lymphatic function improvement after advanced pneumatic compression device treatment of lymphedema. Biomed. Opt. Express 1 (2010), 114-125
12. Lacomba, MT, MJ Yuste Sanchez, AZ Goni, et al: Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: Randomised, single blinded, clinical trial. BMJ 340 (2010), b5396 .
13. Moseley, AL, CJ Carati, NB Piller: A systematic review of common conservative therapies for arm lymphoedema secondary to breast cancer treatment. Ann. Oncol. 18 (2007), 639-646.
14. Herpertz, U: Manuelle Lymphdrainage und Physikalische Odemtherpie. Krankenheits Lehre. Unterrichtsmaterial. Band 3, 1995.
15. Kurz, I: Lehrbuch der Manuelle Lymphdrainage nach Dr. Vodder. Band 3. Krankenheits Lehre, 4, Heidelberg: Karl F. Haugg Verlag, 1989.
16. Cheville, A: Prevention of lymphoedema after axillary surgery for breast cancer. BMJ 340 (2010), b5235.
18. The diagnosis and treatment of peripheral lymphedema. 2009 Consensus Document of the International Society of Lymphology. Lymphology. 2009;42(2):51-60.
19. Lawenda BD, Mondry TE, Johnstone PA. Lymphedema: a primer on the identification and management of a chronic condition in oncologic treatment. CACancer J Clin. 2009;59(1):8-24
20. Rinehart-Ayres, M, K Fish, K Lapp, et al: Use of compression pumps for treatment of upper extremity lymphedema following treatment for breast cancer: A systematic review. Rehab. Oncol. 28 (2010), 10-18.
