SHORT TERM, MID TERM AND LONG TERM EFFECT OF OSTEOPATHIC MANUAL THERAPY (OMT) ON OXYGEN SATURATION IN COPD PATIENTS WHEN COMPARED TO CONVENTIONAL CHEST EXERCISES : Harish s Krishna * Ivor Peter D’Sa * * Vishnu Sharma *** Himavivekanandan ****
ABSTRACT
Background : Chronic obstructive pulmonary disease is a global health concern and is major cause of chronic morbidity and mortality worldwide. Musculoskeletal changes in COPD are characterized by limitation in thoracic expansion with loss of mobility and movement at costochondral, costotransverse and costovertebral joints, tightness and spasm of intercostal muscles. Objectives: Aim of the present study was to study the immediate effect of osteopathic mobilization of ribcage on oxygen saturation in patients with COPD.
Methods : 105 males of age group 45 to 70 years who had at least a year history of COPD were divided in to two groups. One group was given osteopathic manual therapy(OMT) technique (65nos)and the other group received conventional home based chest expansion exercises(40nos), intensive spirometry, upper extremity mobilisation exercises. Oxygen saturation was measured using pulse oxymeter post intervention at 30 minutes(short term), post 24 hours(midterm) and 3 months (long term)post.
Results : The values obtained were statistically analysed using the t- test. There was a significant reduction in oxygen saturation in both groups in short term and midterm, but the saturation level improved significantly in long term. There was no significant difference between the improvements among the groups. Conclusions: Osteopathic Manual Therapy technique and conventional exercises are useful in improving oxygen saturation in patients with COPD but there is no difference seen between the two groups.
Keywords :COPD, Conventional exercises, Osteopathic manual therapy, Oxygen saturation.
INTRODUCTION
COPD is the limitation of airflow that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lungs to noxious particles, gases. Chronic airflow limitation characteristic of COPD is caused by a mixture of small airway disease (obstructive bronchiolitis) and parenchymal destruction (emphysema), the relative contribution vary from person to person”- the global initiative for chronic obstructive lung diseases (GOLD).
Exposure to tobacco smoke is most significant risk factor of chronic obstructive pulmonary disease. The second most risk factor is alpha antitrypsin deficiency and certain occupational exposures.
Chronic obstructive pulmonary disease is a global health concern and is major cause of chronic morbidity and mortality worldwide. American thoracic society has defined COPD as a disease state characterized by the presence of air flow limitation due to chronic bronchitis, emphysema, bronchial asthma and bronchiactasis, the air flow obstruction is progressive may be accompanied by airway hyper reactivity and may be partially reversible versible Chest physical therapy has an important role in a medical team to assist in resolving critical problems deriving from COPD. The goals of Chest physical therapy in COPD are- clearance of excess secretions, prevention of lung atelectasis and improvement of chest mechanics.
Physical therapy for chronic obstructive pulmonary disease basically aims to relieve bronchial obstruction by postural drainage with percussion, positioning, breathing exercise, autogenic drainage, active cycle of breathing etc. Among the various techniques used as interventions the thoracic lymphatic drainage with and without activation is the vast studied one. Thoracic lymphatic drainage helps in relieving bronchial obstruction as well as reducing residual volume of lungs. In addition to that it helps in better lymphatic drainage. Reviews show the next aim for chest physical therapy is to counteract the musculoskeletal changes in COPD.Musculoskeletal changes in COPD are characterized by limitation in thoracic expansion with loss of mobility and movement at costochondral, costotransverse and costovertebral joints, tightness and spasm of intercostal muscles.
Oxygen saturation refers to the extent to which haemoglobin is saturated with oxygen. Hemoglobin is an element in the blood that binds with oxygen to carry it through the blood stream oxygen saturation level usually measured through pulse oxymeter and is normally 95- 100%. In patients with COPD, however the oxygen saturation level leads to drop below normal, especially where they are exerting themselves.
To check the devastating complications of COPD which adversely affects the lung function, different treatments should be well coordinated to improve lung expansion by increasing the rib cage mobility.Use of osteopathic mobilization of rib cage(cost vertebral and thoracic facet joints) and intercostals muscle stretching for COPD has a long tradition among osteopathic professionals but remains a novel approach in the larger biomedical community. Only a very few a studies have attempted to measure the effect of such procedures in pulmonary function tests.(journal of manipulative physical therapy). Even though the patients undertook osteopathic treatment for COPD reported reduce work of breathing and the immediate effects of the techniques are contradictory. Various studies proved that the residual volume of the lungs were more when checked within 30 minutes after the treatment.
Traditional CPT s an invariable component is thoracic lymphatic drainage. This technique has been extensively studied and used by treating physicians and physical therapists. The technique was first described by Miller in 1927.It was specifically developed to improve the antibody response in the body through increased lymphatic flow, to improve the forced expiration ratios. The immediate effects of thoracic lymphatic drainage without activation and osteopathic techniques (rib cage mobilization, intercostals muscle stretch)according to an extensive literature review are found to be contradictory. The immediate effects of thoracic lymphatic drainage without activation and osteopathic techniques (rib cage mobilization, intercostals muscle stretch) on lung function s were not studied separately. The aim of the study was toinvestigate the immediate(30 minutes) effect of osteopathic manual therapy and conventional treatment on oxygen saturation among chronic lung disease patients.
MATERIALS AND METHODS:
105 Subjects were selected from the population group satisfying the inclusion criteria from the patients of the department of general medicine, respiratory medicine of AJ hospital and research centre, and two old age homes in Mangalore by using purposive sampling. Informed consent was obtained from the subjects before recruiting in the study. The subjects were randomly assigned to two group: Group A (Intervention group, subjects who receives OMT) and Group B. (control group,subjects who receive conventional treatment). The subjects of intervention group received the osteopathic manual therapy (OMT) and the control group received conventional chest expansion exercises, incentive spirometry, and upper extremity mobilization exercises.Pre and immediate post treatment oxygen saturation was measured using a finger pulse oximetry (OXYCHECK tm). The inclusion criteria for the study were males between age group 45-75 years, with minimum of one year history of chronic lung disease. (Referred by the pulmonologist). The subjects with acute illness, infections, fracture- rib/ thoracic vertebrae, other permanent orthopaedic chest wall/ thoracic vertebral deformities were excluded from the study.
OMT application technique:
Patient was asked to sit erect without back support at the edge of the bed. The therapist s arm supported the patient s head and neck from anterior for upper 3 thoracic spines andtherapist’s trunk supported the patient s body from behind. For mid and lower spine movements the anterior support was given over the sternum by keeping a roll of cloth between the support hand and the sternum. Using thumb and Vgrasp the therapist performed graded P-A glides (small and large amplituderhythmic oscillations at the beginning and at the end of the range)through thespinous process of the first till 12th thoracic vertebrae.13
Rib glidings.
The therapist stood behind the patients and supports subject s left trunk. The web space of the therapist s right hand contacts the posterior border of the right first rib. The therapist’s hand is rolled slightly backward to position the trapezius muscle out of the way. While the therapist’s left arm supports patients head and neck, move through an arc of flexion and extension to locate neutral position. The therapist’ s right arm guides a right to left translator movement at T1 while concurrently gently right side bending the patients neck, which encourages left rotation at T1. Thepatient was asked to take a deep breath and exhale. During exhalation the therapist provided small amplitude rhythmic oscillations at the beginning of the range. The same procedure was repeated for the left side.13

Subject was made to sit at the edge of bed, therapist stood behind the patient. The therapist grabs the patient’s right upper extremity, therapist s right hand thumb and index finger glides over the lower ribs in cranial direction with inspiration. The movement was held for 7-10 seconds and repeated several times.
Conventional breathing and chest expansion exercises, upper extremity ROM exercises: This included the following exercises –
1. Diaphragmatic breathing exercise
2. Segmental breathing exercises- lateral costal expansion, posterior basal expansion, lingual expansion, apical expansion,
3. Side bendings with inspiration, trunk rotations with inspiration.
4. Upper extremity abduction, flexion with inspiration and expiration.
5. purse lip breathing
6. Incentive spirometry
The subject was seated in semi upright position. The patient was asked to take 3 to 4 slow easy breathes and maximally exhale the fourth breath. The spirometer was then placed in the mouth and the patient was asked to maximally inhale through the spirometer and hold the inspiration for several seconds. The patient was asked to repeat it 5 to 10 times per day.
DATAANALYSIS:
Following statistical formulae were used for data analysis:
Mean which is the simplest measure of central tendency. Standard deviation is defined as the square root of the average of square deviations. Unpaired t -test is applied to unpaired data of independent observation made on individuals of two different or separate groups or sample drawn from two populations.Paired t-test is applied to paired data of independent observation from one sample only when each individual gives a pair of observations.
RESULTS:
MEAN VALUES
Table-1/ graph-1
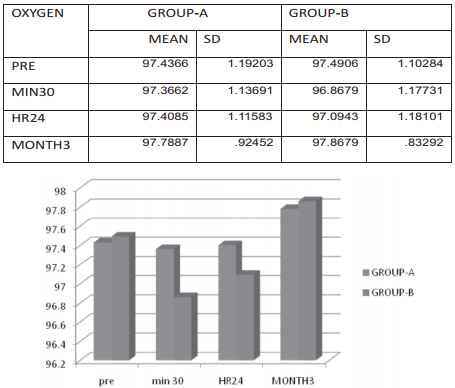
For gr-A- the mean values decreased slightly post 30min of treatment and continue to increase 24 hours post and 3 months post. For gr-B- the mean value has decreased significantly after 30 minutes and increased after 24 hours and 3 months. For both the groups the mean values reduced immediately after treatment.
PRE POST COMPARISON-GROUP-A
Table Graph – 2
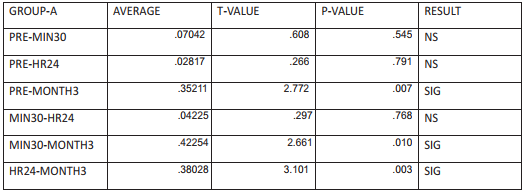
THE GRAPH SHOWS THE AVERAGE OF MEAN DIFFERENCE IN OXYGEN SATURATION
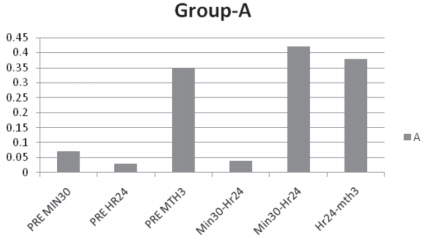
For group-A even though the saturation Pre- 30 min post- the values decreased ,but its not statistically significant, which again continued so fromPre- 24 hrs post. But Pre- 3 months post- there is a significant improvement in saturation.
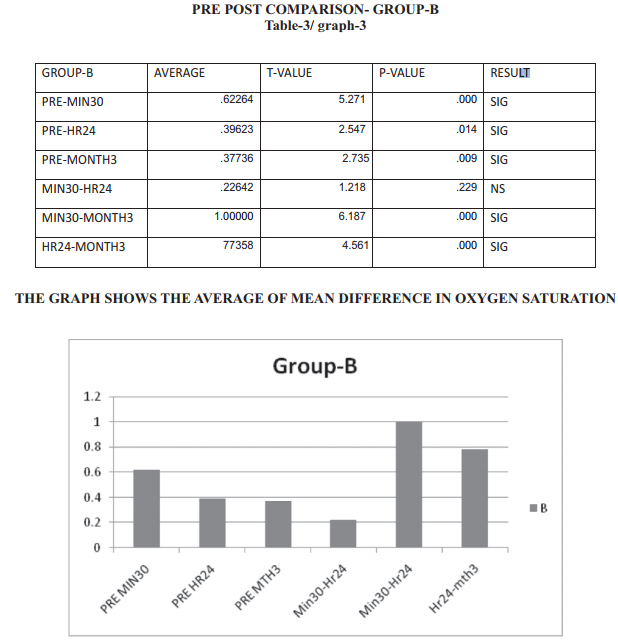
With in group difference
In group-B Pre- 30 min post there was a significant reduction in saturation and continued so during Pre- 24 hours, but better than 30 min post.Pre- 3 months post- there is a significant improvement in saturation.
BETWEEN GROUP COMPARISON
Table-4/graph-4
The Graph Shows The Comparison Ofaverage Mean Difference In Oxygen Saturation Between The Groups.
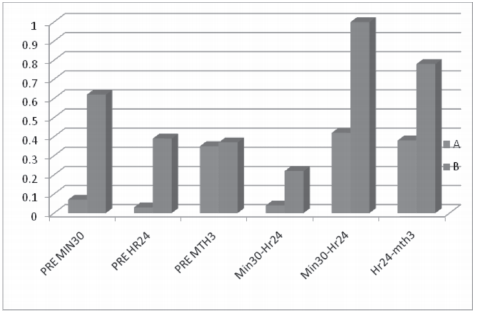
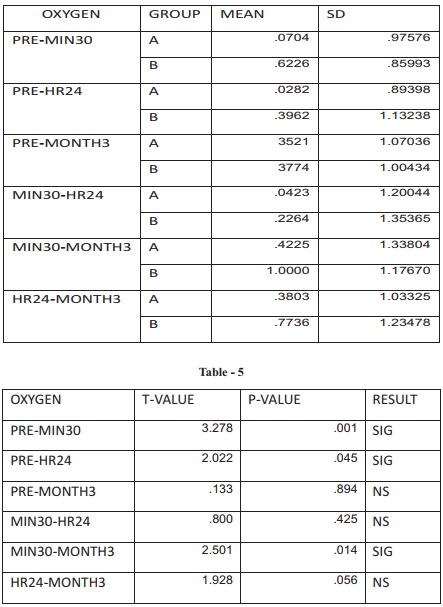
Between group differencePRE-
30 MIN POST and Pre- 24 hours post – both groups the values decreased but gr-A s reduction is not significant when compared to group-B. Pre- 3 months – both groups the value increased considerably but no difference between the groups.
Discussion
COPD is a condition which has many systemic manifestations. The correlation of COPD with changes in blood pressure, heart rate and respiratory rate is well documented. The baro and chemoreceptors which alerts during hypoxemia and hypercapnia is less responsive in COPD patients. The saturation level in COPD patients are maintained by an elevated respiratory rate.The saturation fell down drastically in both groups after the session.when compared the fall was more with conventional group. The fall in saturation is best explained with exercise induced spasm which happened with both treatments. All the patients undergone the study reported an elevated breathing strain immediately after the treatment , which disappeared later. This is common after chest mobilizations and breathing exercises. but there was no additional benefits reported for patients undergone OMT session. Both the groups had a better saturation level than pre sessions after 3 months of regular exercises. when compared between the groups the conventional treatment group s saturation level was better when compared to OMT group. This study explains the benefits of regular breathing exercises for COPD.
Conclusion
The study was initiated to understand the effectiveness of osteopathic manual therapy in COPD patients. It is done in 105 patients in two groups one undergone OMT sessions, second with conventional physical therapy breathing exercises. oxygen saturation was measured prior to session, 30 minutes,24 hours, and 3 months post treatment sessions. For both the groups saturation fell down immediately after the session, but the conventional group s reduction was more than OMT ones.and regained by 24 hours and by 3 months of regular rehabilitation. Even though the saturation level was better than the pre session readings for both the groups,the conventional group s level was better than OMT one. This study shows the effectiveness of regular exercises in the betterment of COPD patients.
References
1. The Global Initiative for Chronic Obstructive Lung Disease: Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Gig Harbor, WA: MedicalCommunications Resources, Inc; 2009.
2. Celli BR. Update on the management of COPD. Chest. 2008;133(6):1451-1462.
3. Anthonisen NR, Skeans MA, Wise RA, Manfreda J, Kanner RE, Connett JE. The effects of a smoking cessation intervention on 14.5-year mortality. Ann Intern Med. 2005;142(4):233-239.
4. Jennifer A, Pryor SAP. Physiotherapy for respiratory and cardiac problems: adults andpaediatrics (pp 143-73). London: Churchill Livingston, 2008.
5. Leelarungrayub D, Pothongsunun P, Yankai A, Pratanaphon S. Acute clinical benefits ofchest wallstretching exercise on expired tidal volume, dyspnea and chest expansionin a patient with chronic obstructive pulmonary disease: a single case study. J BodywMovTher 2009;13:338-43.
6. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al.; ATS/ ERS Task Force. General considerations for lung function testing. EurRespir J 2005a;26;153-61
7. Becklake, M. R., Mcgregor, M., Goldman, H. I. And Braijdo, J. L. A study of the effects of physiotherapy in chronic hypertiophicemphysemausinglung function tests. Dis. Chest, 26: 180, 1954
8. MILLER, W. F. A physiologic evaluation of the effects of diaphragmatic breathing training in patients with chronic pulmonary emphysema.Am. J. Med., 17: 471,1954.
9. HAAS, A. and LUCZAK, A. K. The Application of Physical Medicine and Rehabilitation to Emphyscma Patients. New York, 1963.
10. LEUALLEN.E . C. and FOM~LERW. . S. Maximal midexpirato.ry flow. Am. Rev. Tiberc., 72: 783, 1955.
11. BOREN, H. G., KORY, R. C. and SYNER, J. C. The Veterans Administration-Army Cooperative study of pulmonary function. Am. J. Med., 41: 96, 1966.
12. Patel IS, Seemungal TA, Wilks M, Lloyd-Owen SJ, Donaldson GC, Wedzicha JA. Relationship between bacterial colonisation andthe frequency, character, and severity of COPD exacerbations. Thorax 2002;57:759-64.
13. Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2006, Issue 4.
14. Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A selfcomplete measure of health status for chronic airflow limitation. The St. George’s respiratory questionnaire. Am Rev Respir Dis 1992;145:1321- 7.
15. Williams JE, Singh SJ, Sewell L, Guyatt GH, Morgan MD. Development of a self-reported chronic respiratory questionnaire(CRQ-SR). Thorax 2001;56:954-9.
16. Mahler DA, Weinberg DH, Wells CK, Feinstein AR. The measurement of dyspnea. Contents, interobserver agreement, andphysiologic correlates of two new clinical indexes. Chest 1984;85:751-8.
17. Morgan MD. Preventing hospital admissions for COPD: role of physical activity. Thorax 2003;58:95- 6.
18. Buys EM, van Hemel NM, Kelder JC, Ascoop CA, et al. Exercise capacity after his bundle ablation and rate response ventricularpacing for drug refractory chronic atrial fibrillation. Heart 1997;77:238-41.
19. Redelmeier DA, Bayoumi AM, Goldstein RS, Guyatt GH. Interpreting small differences in functional status: the sixminute walk test in chronic lung disease patients. Am J RespirCrit Care Med 1997;155:1278-82. (LCADL). Respir Med 2002;96:725-30.
20. Ries AL. Pulmonary rehabilitation and COPD. SeminRespirCrit Care Med 2005;26:133-41. 21. Cambach W, Chadwick-Straver RV, Wagenaar RC, van Keimpema AR, Kemper HC. The effects of a community-based pulmonaryrehabilitation programme on exercise tolerance and quality of life: a randomized controlled trial. EurRespir J 1997;10:104-13.
