TENNIS ELBOW – EFFECTS OF ELBOW MWM ON SHOULDER ROM : Shekhar Singh *
Abstract
Clinical observations have suggested a relationship between shoulder range of movement (ROM) and lateral epicondylalgia. This study reports the effect of an intervention of a mobilization with movement (MWM) applied to the elbow, on shoulder rotation ROM in subjects with lateral epicondylalgia. Thirty two subjects with lateral epicondylalgia were included. In a one-group pretest-post-test design, ROM of shoulder internal and external rotation were measured by goniometer before and after the application of the MWM, of both the unaffected and the affected limbs.
Significant differences in pre-intervention external rotation ROM were found between unaffected and affected shoulders of subjects with lateral epicondylalgia, but no significant difference remained post intervention.
It may be concluded that restriction of shoulder rotation ROM is present in patients with lateral epicondylalgia, probably due to a facilitated level of shoulder rotator muscle tone. Shoulder internal and external rotation ROM increases significantly following MWM to the elbow, in subjects with unilateral lateral epicondylalgia.
These findings suggest that the MWM causes a neurophysiologically mediated decrease in resting muscle.
Introduction :
Lateral epicondylosis (LE) is the most common complaint with complex aetiological and pathophysiological factors on the lateral side of elbow. It is characterized by pain at the lateral aspect of the elbow, commonly associated with resisted wrist or finger extension and gripping activities (Noteboom, Cruver, Keller, Kellogg, & Nitz, 1994; Stephens, 1995; Vicenzino & Wright, 1996). LE is also known as lateral epicondylitis, lateral epicondylalgia, tennis elbow, or tendinitis of the affected forearm extensor muscles (e.g. extensor Carpi radialis brevis tendonitis) (Bisset et al., 2007; Vicenzino & Wright). It affects 1–3% of the adult population, occurs mainly as episodes in the dominant arm of patients aged 35–50 years, and is equally distributed between men and women (Smidt et al., 2002; Stratford & Levy, 1994).
Mobilization with movement (MWM) is a system of manual therapy interventions developed by Brian Mulligan that combine a sustained manual `gliding’ force to a joint with concurrent physiologic (osteokinematic) motion of the joint, either actively performed by the patient, or passively performed by the operator (Mulligan 1992, 1993, 1995). The manual force, or mobilization, is theoretically in- tended to cause repositioning of `bony positional faults’ (Mulligan 1993). The intent of MWMs is to restore pain-free motion at joints that have painful limitation of range of movement (ROM) (Mulligan 1995).
The specific manual therapy intervention utilized in this study is the `MWM for tennis elbow’ described by Mulligan (1992, 1995, 1999) The technique used in this study is fully described in a previous paper (Abbott et al. 2001). In some severe cases, a variable degree of deficit of elbow ROM may be seen (Noteboom et al. 1994). The presence of a difference in shoulder ROM in patients with LE has not previously been reported. A change in shoulder ROM following a manual intervention to the elbow has been previously reported, by the primary investigator of this study (Abbott 1998). A deficit in shoulder ROM may have implications regarding intervention, particularly in occupational health. A change in shoulder ROM following manual therapy to the elbow would suggest that pre-intervention limitation was not a mechanical limitation, but rather was neurophysiologic in nature.
Prevalence of the disorder ranges from 2.8% in the general population with increases up to 7.4% in the engineering industry. Despite being widely known as tennis elbow, more cases can be attributed to mechanical stress related to occupation than to tennis. The irony of this disease is that only 5% to 10% of those with “tennis elbow” actually play tennis. Peak incidence occurs between 45–54 years of age with the dominant arm typically affected. Some indicate that LE has been described as a self-limiting condition with 89% of those diagnosed reporting decreases in pain at 1 year, whereas others have estimated as much as 40% of those diagnosed experience prolonged symptoms leading to impaired function. In tennis the injury risk was fairly similar for males and females. In most patients aged over 30 the condition may be considered to be a degenerative process, the onset of symptoms being hastened by overuse of the arm.
In case of Tennis elbow active movement causes repeated breakdown in the formation of scar tissue, which subsequently prolongs the inflammatory reaction and leads to the formation of adhesions. Current evidence following surgical intervention indicates that LE is a chronic disorder demonstrated by the presence of degenerative changes, such as increased fibroblasts and disorganized collagen, as opposed to inflammatory cells. These findings are contradictory to the widely used term epicondylitis, which describes an inflammatory condition. It has recently been recommended that the term epicondylitis be replaced with epicondylosis, a more accurate descriptor of the underlying degenerative process, or the generalized term eicondylalgia.
Although the etiology of tennis elbow is unclear, the primary factor is most likely to be a mechanical predisposition of the elbow associated with a force overload. Cabot believes that acute lateral epicondylitis has an inflammatory basis involving parts or all of the extensor tendon aponeurosis . Chronic lateral epicondylitis however is caused not only by the inflammation in the extensor tendons but also by contracture of the anterolateral elbow capsule.
The treatment of tennis elbow is often a frustrataing experience for the clinicians due to the frequent failure of obtaining a symptomatic improvement in the patient. This failure is equally apparent in both conservatively & surgically treated patients. Therefore the management of tennis elbow both at early and late stages has been suggested to be primarily a conservative approach . It is therefore important to substantiate an effective, noninvasive, conservative therapy for this disabling affliction. A wide array of physiotherapy treatments have been recommended for the management of LET.
One particular manipulative therapy technique that has been receiving considerable attention in the literature in the management of LE is Mulligan’s Mobilization with Movement (MWM). The MWM technique is a non-thrust manipulative technique performed in the following fashion: The therapist first identifies a physical activity that the patient reports to be painful. Most often this entails the patient clenching the fist, a task that is frequently impaired in LE. The patient is next instructed to perform the identified painful task while the therapist provides a laterally directed glide to the elbow. Preliminary findings have suggested that the orientation of the lateral glide and the amount of manual force applied by the therapist is critical to the effective application of this technique. Directing the lateral glide force somewhat posterior or directly lateral is most effective. The MWM is typically repeated for 6 to 10 repetitions per visit and then repeated over several follow-up sessions. Perhaps most critically, the MWM should be repeated as part of a home exercise program between physical therapy visits.
The purpose of this study was to establish whether a difference exists between the shoulder internal or external rotation ROM of the affected extremity versus the unaffected extremity of persons with LE and the shoulder internal or external rotation ROM of the affected extremity of persons with LE improves after the application of the MWM.
METHODS
Subjects were recruited from those included in a trial of the effect of MWM on LE symptoms and grip strength (Abbott et al. 2001). Exclusion criteria included persons who had a) bilateral lateral epicondylalgia; b) surgery for lateral epicondylalgia within the last twelve months; c) history of fracture of either humerus, radius or ulna that they knew to limit ROM; d) history of shoulder surgery that they knew to limit ROM; or e) history of rheumatoid disease, or f)neurologic impairment including stroke or head injury. Also excluded were subjects who responded negatively to the MWM trial (Abbott et al. 2001). Elimination of subjects who respond negatively to the MWM trial is consistent with established principles of clinical decision-making in the application of all mobilizations with movement (Mulligan 1993, 1995; Vicenzino & Wright 1995).
Materials
A gravity-dependent goniometer (Johnson Industries, USA) was used for the shoulder ROM measurements.
Reliability
Intratester reliability assessment of goniometric measurement of shoulder internal and external rotation was performed prior to the commencement of data collection for this study. Thirty trials of each measurement (three trials on each of ten normal volunteers) were performed by the investigator, who was unable to see the face of the goniometer. The goniometer was read by the research assistant. Intraclass correlation coefficients were high for both internal rotation (0.98) and external rotation (0.92), indicating excellent reliability of repeated measures. The standard error of measurement (SEM) was estimated to be 2.54 degree for internal rotation and 3.09 degree for external rotation.
Procedure
The research protocol is summarised as follows:
1. Subjects signed a consent form to participate in the study, and completed a brief questionnaire
2. Subjects were instructed to lie supine on a treatment table. The comparable sign movement was established (Abbott et al. 2001)
3. By random assignment, either the left or right arm was designated to be tested first.
4. Goniometric measurement of passive shoulder internal and external rotation ROM was performed (Norkin & White, 1995). The investigator performed the goniometry, but was unable to see the face of the goniometer, which was read and recorded by the research assistant. The end-point of ROM was considered to be that reached by gravity alone, without overpressure applied by the investigator. Both limbs were measured in the same manner, in the order dictated by random assignment.
5. The investigator performed the MWM to either the left or the right elbow (according to the random assignment). On the unaffected side the patient performed the same movement that would have reproduced elbow pain on the affected side. Based on the suggestion of Mulligan (1995), the patient performed motion up to ten times while the MWM was being applied. If the pain returned prior to achieving ten, no further repetitions were performed.
6. The limb tested was re-measured for gonio-metric ROM
7. The investigator performed the MWM to the remaining elbow, and subsequently re-measured the ROM of that shoulder. Total subject time was approximately 15 min.
Data analysis
The shoulder rotation ROM goniometry data are matched samples (pre-post, or affected unaffected). The one-tailed t-test was used to compare group means, as clinical observations indicated a unidirectional effect of the intervention on the dependent variables. The statistical package used for data analysis was SPSS 21.0 (SPSS Inc., Chicago, Ill., USA). The a priori level of significance was set at a=0.05. Although the SEM would allow lower, clinical significance for goniometric ROM was set at the more conservative standard of 58 (Boone et al. 1978; Boon & Smith 2000).
Results
Thirty-two subjects were referred for this study. Six subjects were ineligible (two with bilateral epicondylalgia, one with medial epicondylalgia, one without a comparable sign, and two with a negative response to MWM). Two subjects declined to participate in the study, and one potential subject was unable to be contacted. The twenty-three subject who fulfill the inclusion & exclusion criteria were included in this study. Subjects had experienced LE for an average of sixteen months.
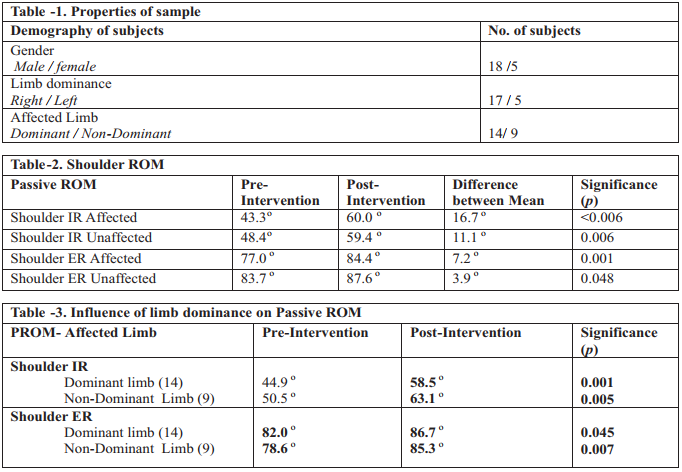
Analysis by the w2 test confirmed that the distribution of the data was not significantly different from that designed by the normal curve. The t-test was, therefore, able to be used to obtain the following results. Shoulder rotation range of motion Means for preintervention and post-intervention ROM are provided in Table 1. Pre-intervention, shoulder external rotation range of motion of the affected limb was significantly less than that of the unaffected limb (P=0.038) (Table 2). The pre- intervention difference in internal rotation between the affected and unaffected limbs was not statistically significant (Table 2). Post-intervention, shoulder rotation ranges of motion for the affected limb versus the unaffected limb were not significantly different (Table 2)
DISCUSSION
This study was of a one-group repeated measures design. Because the study does not include a control group, it is considered a quasi-experimental design (Portney &Watkins 1993), and as such it has inherent limitations. Threats to internal validity, such as maturation or history effects, and treats to external validity, such as sample bias, are limitations inherent to this design. This design was chosen, however, because threats to internal validity were minimised by completing the data collection within a single testing session (Portney & Watkins 1993)
Normative values for shoulder rotation ROM may have provided a useful comparison, however the literature does not provide normative values for a comparable demographic, using a similar scapulastabilised goniometric method (Norkin & White 1995; Boon & Smith 2000).
Deficit in affected limb shoulder rotation range of motion:
In this group of subjects with lateral epicondylalgia, the affected limb demonstrated a deficit in external rotation ROM, compared to the unaffected limb, prior to intervention. This effect cannot be explained by an effect of limb dominance, as analysis of shoulder external rotation of the dominant limb versus the non-dominant limb, regardless of side of LE, demonstrated no significant difference.
It is possible that either the deficit of ROM came first, and led to the LE, or that the LE came first and caused a decrease in shoulder ROM. The author speculates that the latter is true; given that the data indicate that the shoulder external rotation ROM was normalized post-intervention (i.e. rotation ROM of the affected shoulder was not different to that of the unaffected shoulder post-intervention, whereas prior to intervention the measures were different). The initial limitation of shoulder external rotation ROM noted in this group of subjects may be due to facilitated muscle activity of the shoulder musculature, as a response to distal symptoms. This view is supported by the finding of greater ROM post intervention. It was identified that injuries to an animal’s limb causes facilitation of not only the muscles crossing that area, but also muscles remote to the injured area. Several other investigators have reported facilitated muscle activity due to musculoskeletal injury, either locally or remote to the area, in both humans and animal models (Johansson & Sojka 1991; Ben-Yishay et al. 1994; Indahl et al. 1995; Indahl et al. 1997; Hall et al. 1998).
Intervention to the elbow causes an increase in shoulder rotation range of motion:
Non-contractile (i.e. capsular, ligamentous, fascial, or bony) limitation of the shoulder would not be mechanically affected by a technique to a distal joint that leaves the shoulder rested in a static, loose-packed position throughout the procedure. Several studies have documented the neurophysiologic effects of manual therapies (Sullivan et al. 1991; Vicenzino et al. 1994; Vujnovich & Dawson 1994; Murphy et al. 1995). The presence of elbow pain may elevate the level of facilitation of the motor-neurone pool in the spinal cord, either by direct neuronal pathways within the spinal cord, or via the cortex. MWM eliminates the elbow pain (Abbott et al. 2001), which would hypothetically reduce any abnormal facilitation, allowing the motor-neurone pool to return to a lower level of excitation.
CONCLUSION
A manual therapy technique to the elbow significantly changed internal rotation and external rotation ROM of the shoulder, in patients with unilateral lateral epicondylalgia, both on the affected side and the unaffected side. External rotation range of motion of the shoulder was significantly limited in patients with unilateral lateral epicondylalgia. It is theorized that limitation of shoulder ROM was due to facilitated muscle activity of the shoulder musculature, and that the MWM reduces this level of facilitation, thus allowing increased shoulder ROM.
References:
1. Noteboom T, Cruver R, Keller J, Kellogg B, Nitz AJ 1994 Tennis elbow: A review. Journal of Orthopaedic and Sports Physical Therapy. 19(6): 357-366.
2. Vicenzino B, Collins D, Wright T 1994 Sudomotor changes induced by neural mobilisation techniques in asymptomatic subjects. Journal of Manual and Manipulative Therapy 2(2): 66-74.
3. Abbott JH 1998 The effect of elbow mobilisation with movement on shoulder impairment and functional limitation: A case report. Journal of Manual and Manipulative Therapy 6(4): 208.
4. Ben-Yishay A, Zuckerman JD, Gallagher M, Cuomo F 1994 Pain inhibition of shoulder strength in patients with impingement syndrome. Orthopedics 17(8): 685-688.
5. Ashe M, McCauley T, Khan K. Tendinopathies in the upper extremity: Aparadigm shift. J Hand Ther. 2004;17:329-334
6. Bunata RE, Brown DS,Capelo R. Anatomic factors related to the cause of tennis elbow. J Bone Joint Surg Am. 2007 Sep;89(9):1955-63.
7. Cyriax JH. The pathology and treatment of tennis elbow. J Bone Ioint Surg 1936: 18: 921-38
8. Exelby L 1996 Peripheral mobilisations with movement. Manual Therapy 1: 118-126
9. Norkin CC, White DJ 1995 Measurement of Joint Motion: A Guide to Goniometry. FA Davis Company, Philadelphia, PApp62-63.
10. Boon AJ, Smith J. 2000 Manual scapular stabilization: Its effect on shoulder rotational range of motion. Archives of Physical Medicine and Rehabilitation 81: 978-983.
11. Boone DC, Azen SP, Lin C-M, Spence C, Baron C, Lee L. 1978 Reliability of goniometric measurements. Physical Therapy 58: 1355-1390.
12. Portney LG, Watkins MP 1993 Foundations of Clinical Research: Applications to Practice. Appleton & Lange, Norwalk, Connecticut ch 10 pp147-148.
13. Boon AJ, Smith J. 2000 Manual scapular stabilization: Its effect on shoulder rotational range of motion. Archives of Physical Medicine and Rehabilitation 81: 978-983.
14. Ben-Yishay A, Zuckerman JD, Gallagher M, Cuomo F 1994 Pain inhibition of shoulder strength in patients with impingement syndrome. Orthopedics 17(8): 685-688.
15. Hall T, Zusman M, Elvey R 1998 Adverse mechanical tension in the nervous system? Analysis of straight leg raise. Manual Therapy 3(3): 140-146.
16. Johansson H, Sojka P. 1991 Pathophysiological mechanisms involved in genesis and spread of muscular tension in occupational muscle pain and in chronic musculoskeletal pain syndromes: a hypothesis. Medical Hypotheses 35(3): 196-203.
17. Indahl A, Kaigle A, Reikeras O, Holm SH 1997 Interaction between the porcine lumbar intervertebral disc, zygapophyseal joints, and paraspinal muscles. Spine 22(24): 2834-2840.
18. Sullivan SJ, Williams LRT, Seaborne DE, Morelli M 1991 Effects of massage on alpha motoneuron excitability. Physical Therapy. 71(8): 555-560.
19. Vicenzino B, Collins D, Wright T 1994 Sudomotor changes induced by neural mobilisation techniques in asymptomatic subjects. Journal of Manual and Manipulative Therapy 2(2): 66-74.
